Raw milk is milk that has not been pasteurized to kill harmful bacteria. Raw milk can be contaminated with harmful germs that can make you very sick. In fact, raw milk is one of the riskiest foods.

People who get sick from raw milk might have many days of diarrhoea, stomach cramping, and vomiting. Some people might develop severe or even life-threatening diseases, including paralysis, kidney failure, stroke, and even death.
People most at risk from severe food borne illness are adults 65 years and older, children younger than 5 years, and people with weakened immune systems. But healthy people of any age can get very sick after drinking raw milk contaminated with harmful germs.
Surveys from various countries have monitored the presence of different types of pathogens in raw milk, like Campylobacter jejuni, Listeria monocytogenes, salmonella etc. World over, raw milk has frequently been identified as the source of foodborne illness outbreaks.
The prevalence of pathogens in milk is influenced by numerous factors, including farm size, number of animals on the farm, hygiene, farm management practices, milking facilities, season, and others.
Raw milk can be contaminated with pathogens even when sourced from clinically healthy animals. Even milk that appears to be of good quality (ie, low total bacteria count) may contain pathogens.
Milk can get contaminated in these ways:
- Germs from an animal’s poop can get in milk
- Germs from an animal’s skin can get in milk
- Germs in the environment (including the barn and milking equipment) can get in milk
- The dairy animal’s udder can be infected (mastitis)
- The dairy animal can have a disease (for example, bovine tuberculosis)
- Insects, rodents, and other small animals can get in milk
- Conditions in the milk processing plant can be unsanitary
- Cross-contamination from dairy workers can happen—for example, through contact with dirty clothing or boots
Dairy farms are an important reservoir of various foodborne pathogens.
Pathogens are not visible to the naked eye, and measurements of their numbers can take several days to complete, so it can be extremely difficult to determine the safety of raw milk before that milk has been consumed. Occasional testing of raw milk does not guarantee that pathogens are absent from the milk supply on days when no testing is done (e.g., because of possible contamination during a single milking occasion).
Ensuring the safety of raw milk by occasional testing is difficult because of the following:
- Difficulties in having sufficient sampling since contamination of milk may be sporadic, and bacterial loads can vary from day to day (i.e., sampling and testing every day provides more confidence to a claim of safety).
- Bacteria/spores are often associated with the fat phase and are not evenly distributed in milk.
- It is possible that the number of organisms (pathogens) present is too low to be detected by the test method but the numbers may be sufficient to cause illness if the effective dose is low (which is the case for several key pathogens.
- There might have been very low initial numbers of a pathogen, which were below the limits of the test method at the time of sampling, but the pathogen might grow if milk was stored improperly.
- It is impossible to test for every single different type of human pathogen.
A common question is, that how come, a lot of people who have been drinking raw milk for years, and they never got sick?
The presence of germs in raw milk is unpredictable. The number of disease-causing germs in the raw milk may be too low to make a person sick for a long time, and later high enough to make the same person seriously ill. For some people, drinking contaminated raw milk just once could make them really sick. Even if you trust the farmer and your store, raw milk is never a guaranteed safe product. Drinking raw milk means taking a real risk of getting very sick.
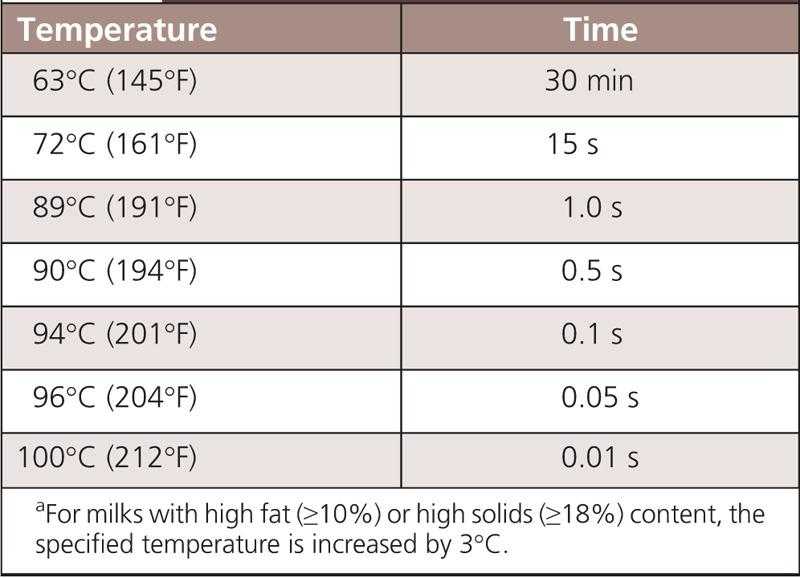
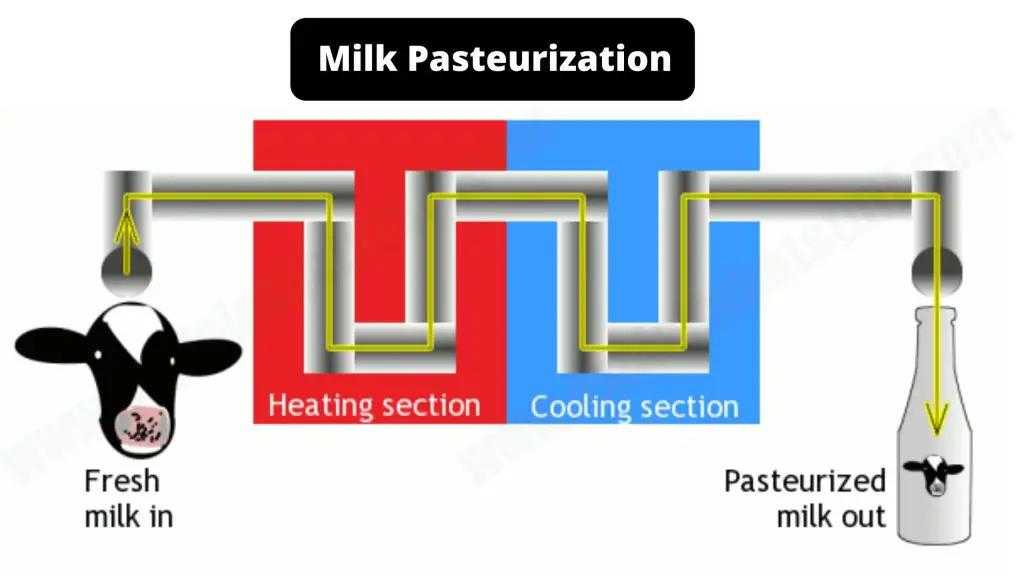
Pasteurization is the process of heating milk to a high enough temperature for enough time to kill harmful germs in the milk. Pasteurization is defined as “the process of heating every particle of milk or milk product, in properly designed and operated equipment, to any 1 of the specified pasteurization time/temperature combinations.”
These time-temperature combinations are designed to destroy all human pathogens, and the most common pasteurization treatment is rapidly heating milk to not less than 72deg C and holding that temperature for at least 15 seconds. In fact, boiling is a much more severe heat treatment than the mild pasteurization process used commercially.
In some countries, milks are subjected to higher (ultra) heat treatments (e.g., 138deg C for 2–4 seconds); if the product is packaged normally, then this milk is called ultra-pasteurized; if the process is done aseptically, then the milk can be stored at ambient temperature, this product is called ultra-high temperature (UHT).
Pasteurization was invented during a time when millions of people became sick and died of tuberculosis, scarlet fever, typhoid fever, and other diseases that were spread through raw milk.
Routine pasteurization of milk began in the United States in the 1920s and became widespread by 1950 as a way to reduce contamination and reduce human illnesses. It led to dramatic reductions in the number of people getting sick. Most public health professionals and health care providers consider pasteurization to be one of public health’s most effective food safety interventions ever.
Some raw milk promoters may claim that there raw milk is well tested. But, negative laboratory tests to detect germs in raw milk do not guarantee that raw milk is safe to drink. Tests do not always detect low levels of contamination. People have become very sick from drinking raw milk that came from farms that regularly tested their milk for bacteria.

Also, whether the cow is grass fed, or milk or 100% organic, raw milk can be contaminated in either case, and pasteurization is needed for all forms of raw milk. Even healthy animals may carry germs that can contaminate milk. Small numbers of bacteria can multiply and grow in milk from the time it is collected until the time a person drinks it. If the milk is not pasteurized to kill germs, people who drink it can get sick.
Even if the cows are kept in absolutely hygienic conditions, the chances of contamination are still there. Illness-causing germs thrive in the environment of dairy farms, even if the farm or barns are kept clean and the farmers are careful when milking. Farmers cannot guarantee that their raw milk and the products made from it are free of harmful germs, even if tests indicate the raw milk does not contain harmful germs.
A number of different claims have been made about the possible health benefits that could hypothetically be derived from the consumption of raw milk. However, there is no reliable scientific evidence to support any of these suggested health benefits:
- Nutritional – During pasteurization, there is no significant change in the nutritional quality of milk. Normal bovine milk contains about 3 to 3.5% total protein. The two major groups of milk protein are casein (about 80%) and whey proteins (about 20%). The protein quality of pasteurized milk is not different from that of raw milk.
Pasteurization does not cause any change in protein quality; minor levels (<7%) of denaturation of whey proteins have been reported due to pasteurization, but protein denaturation has no impact on protein nutritional quality.
Typical bovine milk contains about 3 to 4% milk fat, with 97.5% of the fat existing as triglycerides. Pasteurization has essentially no effect on milk fat composition (saturated, monounsaturated, polyunsaturated).
Pasteurization does not cause any change in the concentrations of minerals; minerals are very heat stable. Pasteurization may cause very minor losses (<10%) of vitamin C, folate (vitamin B9), vitamin B12, vitamin B6, and thiamine (vitamin B1).
Of these vitamins, milk is an excellent source of only vitamin B12; milk has only low concentrations of most of the vitamins listed previously, which might show some minor losses on pasteurization. Pasteurization does not change the concentration of riboflavin (B2) (which is very heat stable) or fat-soluble vitamins like vitamin A or E.
Other factors like type of packaging material, light exposure, and storage time/temperature have much larger impacts on vitamin losses in milk. Feed (like pasture grazing) can greatly influence milk composition, and sometimes proponents of raw milk confuse feed-related changes in milk composition with those caused directly by pasteurization.
Other milk-processing approaches, like ultra-pasteurization and ultra-high temperature, have only a minor impact on the nutritional quality of milk.
A 2011 meta-analysis of 40 studies, assesed the effects of pasteurization on vitamin levels, and concluded that, the effect of pasteurization on milk’s nutritive value was minimal because many of these vitamins are naturally found in relatively low levels.
- Allergy & Asthma – Food allergy is an abnormal immunological response due to sensitization to a particular food (usually a protein). Cow’s milk proteins can trigger an immunoglobulin E–mediated reaction in patients called cow’s milk protein allergy (CMA). Young infants usually outgrow this allergy within the first year of life. Young infants may be more susceptible to CMA owing to their milder digestive systems (weaker pepsin/enzyme activity, higher stomach pH), which exposes them to more allergic responses from “intact” proteins or larger peptide sequences.
In children with CMA, neither raw milk, unhomogenized and pasteurized milk, or homogenized and pasteurized milk was tolerated by CMA patients. It can also be mentioned that dietary intake of pasteurized milk is not correlated with any increased risk of the development of respiratory allergies or atopic dermatitis.
When it comes to Asthma, there have been few studies on the benefit of raw milk consumption. A study, showed that, early life consumption of raw cow’s milk reduced the risk of manifest respiratory infections and fever by about 30%.
However, the study also stated that, if the health hazards of raw milk could be overcome, the public health impact of minimally processed but pathogen-free milk might be enormous, given the high prevalence of respiratory infections in the first year of life and the associated direct and indirect costs. Therefore, the risk to reward ratio is way too high in such cases.
Also, this type of milk is available on a farm setting, that too under proper hygiene conditions. But it’s virtually impossible to mass produce this milk, and transport it to cities, without any fear of contamination.
However, it’s important to note that these studies show an associated risk reduction, not necessarily a direct correlation. Also, the other studies are on farm milk, not raw milk.
There is a common debate on how kids in villages don’t develop these allergies & asthma, and are able to digest milk?
We need to understand the difference between city life & village living. Growing up in a farming environment is associated with a decreased risk of allergy and asthma. Farm kids come into contact with a wider range of bacteria/allergens compared with children who live in modern cities. Early exposure to these farm allergens could help some infants develop a more robust immune system, and have an allergy-protective effect.
Thus, at present, there is no direct evidence of any beneficial impact of raw milk consumption for allergies & asthma.
- Lactose Intolerance – All types of milks (including human or breast milk) contain the sugar lactose, and when we consume milk, the lactase enzyme (Beta-galactosidase) hydrolyses it into glucose and galactose, which are then absorbed by the body. Bovine milk contains app. 4.5% lactose.
Many individuals lose the ability to digest lactose as they age, and they can develop a condition known as lactose intolerance, in which people have digestive symptoms—such as bloating, diarrhoea, and gas—after eating or drinking milk or milk products.
One of the claims made about raw milk is that it does not cause lactose intolerance because it contains lactase secreted by “beneficial” or probiotic bacteria present in raw milk. However, raw milk doesn’t reduce lactose malabsorption or lactose intolerance symptoms compared with pasteurized milk among adults positive for lactose malabsorption.
Because there is no Beta-galactosidase enzyme present in raw milk, there is no obvious reason why raw milk could assist with lactose intolerance. Yogurts, which contain high levels of bacteria that have this β-galactosidase enzyme, are tolerated better by individuals with lactose intolerance.
Although raw milk contains low levels of some proteases and lipases, no physiological role in human digestion has been demonstrated for these enzymes. Both of these are relatively heat stable, so there would be little loss of activity in pasteurized milk relative to raw milk. Anyway, raw milk enzymes are likely degraded/hydrolysed in the human digestion system (due to the stomach acid, pepsin, etc).
- Good Bacteria – Some media reports claim that raw milk is healthy because of the presence of “good bacteria.” Probiotics are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host.” Some lactic acid bacteria are considered probiotics.
Bacteria found in raw milk are not probiotic. Probiotic microorganisms must be non-pathogenic. In contrast, raw milk can host various human pathogens, including E. coli , Salmonella, Streptococcus, Yersinia enterocolitica, Campylobacter jejuni, Staphylococcus aureus, Listeria monocytogenes, Mycobacterium tuberculosis, and Coxiella burnetti to name a few.
There are a number of potential antimicrobial systems in milk, including lactoferrin, lactoperoxidase, lysozyme, bovine immunoglobulin, bacteriocins, oligosaccharides, and xanthine oxidase. Lactoperoxidase and lysozyme retain 70% or more of their activity in pasteurized milk, whereas the other components listed above retain all their activity in pasteurized milk. Collectively, these antimicrobial systems are unable to prevent pathogen growth in raw milk.
- Immunity – many proponents of raw milk proclaim that drinking raw milk over pasteurized, helps strengthen the immune system. However, this is absolutely misleading. Raw milk is not an immune system building food. Children are typically more vulnerable than adults to the pathogens than can occur in raw milk.
The concentration of immunoglobulins in bovine milk is low, typically about 0.6-1.0 mg/ml. At these low concentrations, bovine immunoglobulins, when consumed directly from milk, are physiologically insignificant to humans. Also, these immunoglobulins are quite heat stable and aren’t impacted by pasteurization.
In conclusion, raw milk is not inherently safe and carries a significant food poisoning risk with its consumption. There is no evidence that raw milk has any inherent health or nutritional benefits those media claims were shown to be myths. Pasteurized milk has an excellent food safety record and remains an important dietary source for many important nutrients